Healthcare
Redefining Cancer Nutrition Care Through Culinary Innovation

Find the food and facilities solutions that work best for yours.
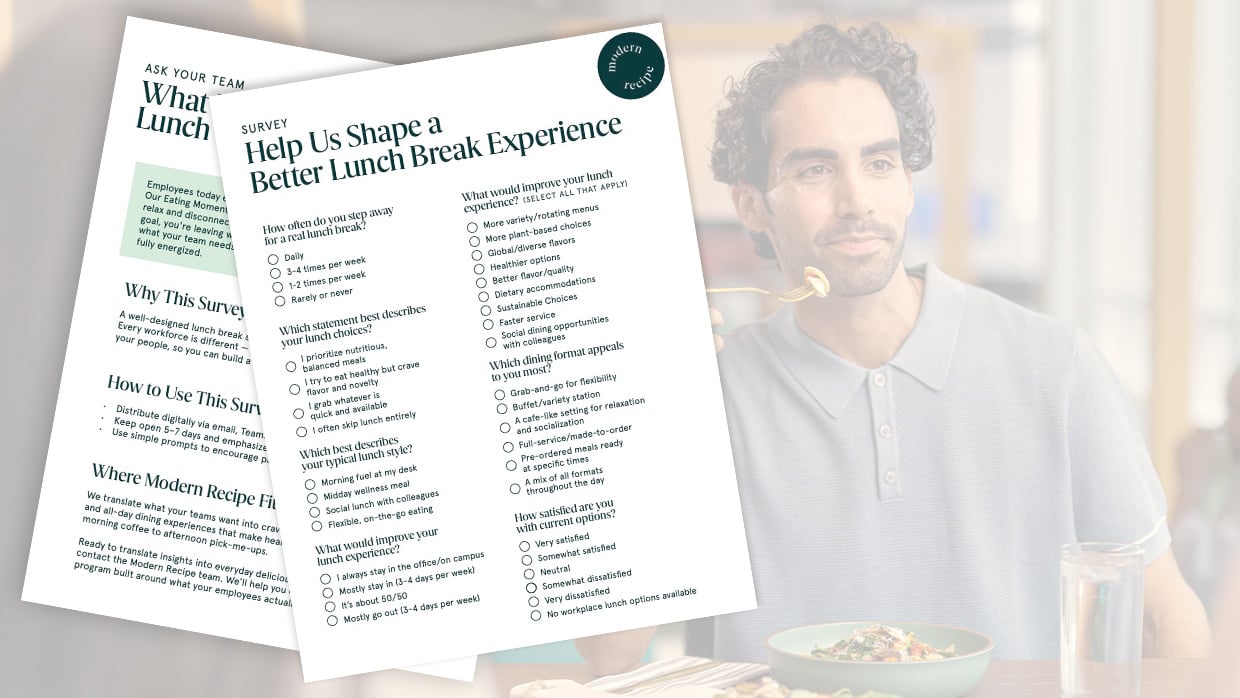
There’s more than meets the eye when it comes to great food in the workplace — it fuels connection, productivity and satisfaction. From energizing breakfasts to social lunches and quick, on-the-go snacks, this study reveals key opportunities to level-up your workplace dining experiences and keep your people happy and productive.
Redefining Cancer Nutrition Care Through Culinary Innovation

Moments of Belonging That Empower Student Success

Debunking 4 Myths About Plant-Based Foods in Schools

The Connection between Employee Nutrition & Performance
Menus that Spark Joy

Award-Winning Chefs Bring James Beard–Inspired Dining to Campus

SUNY Oneonta’s Innovative Internship Programs and Community Collaboration Improve the Perception of Higher Education

The Math–Nutrition Connection: 5 Ways Healthy School Meals Add Up to Better Academic Performance

Innovations in Student-Centered Dining to Support a Growing Campus
