Schools
Debunking 4 Myths About Plant-Based Foods in Schools

Find the food and facilities solutions that work best for yours.
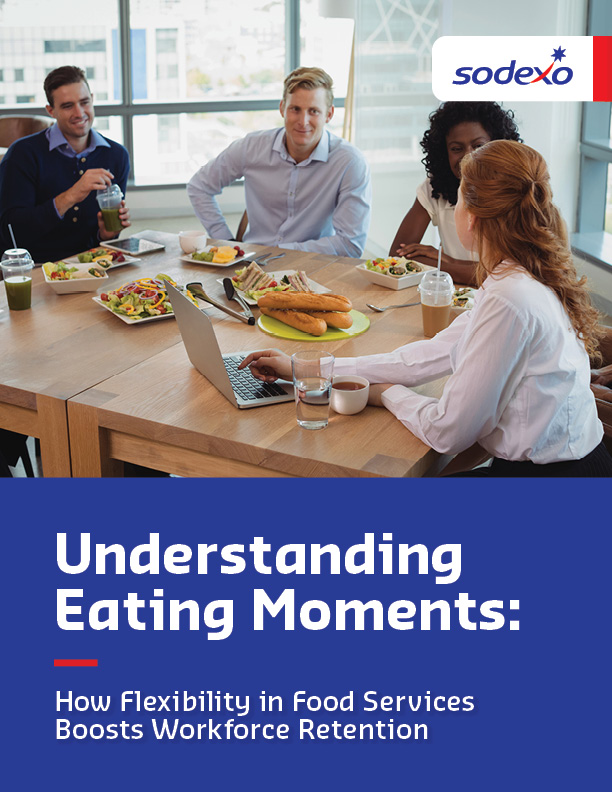
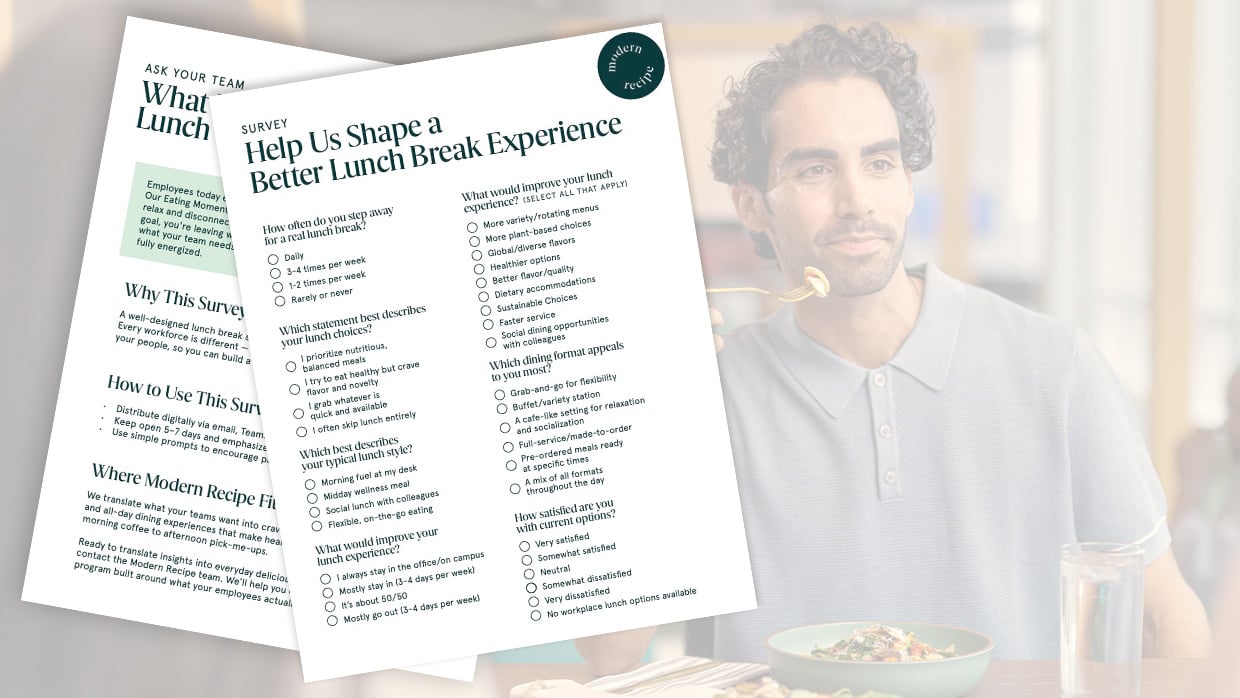
There’s more than meets the eye when it comes to great food in the workplace — it fuels connection, productivity and satisfaction. From energizing breakfasts to social lunches and quick, on-the-go snacks, this study reveals key opportunities to level-up your workplace dining experiences and keep your people happy and productive.
Debunking 4 Myths About Plant-Based Foods in Schools

The Connection between Employee Nutrition & Performance
Menus that Spark Joy

Award-Winning Chefs Bring James Beard–Inspired Dining to Campus

SUNY Oneonta’s Innovative Internship Programs and Community Collaboration Improve the Perception of Higher Education

The Math–Nutrition Connection: 5 Ways Healthy School Meals Add Up to Better Academic Performance

Innovations in Student-Centered Dining to Support a Growing Campus

Celebrating the Best of SUNY Collaboration & Culinary Creativity

Breaking Barriers in Nutrition Care: How a Dietitian Transformed Referrals and Patient Outcomes
